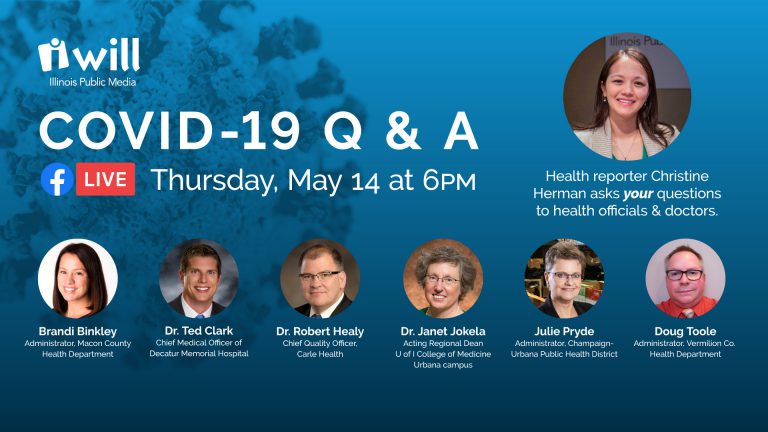
- Status updates from local public health administrators and medical doctors
- COVID-19 immunity, contact tracing, social distancing and face mask guidance
- Antibody testing, advice on reopening the economy, questions about childcare
- Dental care, elective medical procedures, public health services and what’s on the horizon
- Employer responsibilities, where to report issues and final thoughts
Public health services
Christine Herman: I want to shift back to public health just for a moment. Brandi, Melissa has a question. She wants to know if the Macon County Health Department will reopen to the public for services. And what would be the timeline for that?
Brandi Binkley: Well, the health department has actually been available for services throughout the response to this pandemic. Because of the risk associated with some of our services, we did have to either drastically limit those or suspend them temporarily. Certainly call the health department. Let us know if there’s something that you need that we’re not able to provide or that you haven’t been able to access.
But we’ve definitely done everything that we can to still provide all of those essential services. We’re just doing them in different ways, in order to limit the risk of exposure for our staff, and also our clients. So some of our services have been changed to appointment only, some of them have been changed to virtual or over the phone. Some have been converted to curbside services. So we’ve gotten very creative in order to limit the number of people physically coming into our building. But we’re certainly still open and providing services on a very comprehensive basis throughout this time.
Routine dental care resuming
Christine Herman: We got a question about dental care. Some dental offices are planning to open as early as May 11th. Kelsie says, “Do you think that is wise, since barbers and salons are being told to stay closed?” Julie, can you weigh in on this question?
Julie Pryde: The risk there is to the dentist or the hygienist and the assistant and the people that are in the room because dental procedures cause aerosolization. So that would push the virus up into the air.
But the difference between, let’s say, a salon and a dental office, dental care is health care. People need to have dental care, and you know, as lovely as it is not having a haircut as evidenced by me, it’s not a health concern. So the dentists need to get open as fast as they can safely.
Salons are set to open in Phase Three, which the way our region is going, will be at the end of the month or the beginning of the next month. So that’s pretty much the difference. But what’s going to be the limiting factor for dental offices is: Do they have enough of the personal protective equipment to do it safely? And right now, there’s still a shortage. So the dentists are going to need assistance, just like everyone else, getting that personal protective equipment.
Christine Herman: Doug, is there anything else you would add to that when it comes to dentist offices in Vermillion County, trying to figure out whether and how to reopen safely and resume routine dental care?
Doug Toole: I think Julie covered it very well. I imagine it’s going to start with an appointment-only basis for those with the most severe need to get into see the dentist. And we’ll start to move back into the routine stuff later.
Christine Herman: And Dr. Healy, as a primary care doctor, do you advise people to call if they’re concerned or have questions about as they’re trying to weigh the risks versus benefits of going in for a dental procedure? And how would you walk people through that process of figuring that out?
Dr. Robert Healy: Your primary care doctor, knowing you, will be able to talk to you about what your health risks are. And similar to what we talked about with going out into a group of 10 and more as we go further down the path to getting back to normal, I think it’s important to know what your own risks are.
So your provider can tell you, if you have diabetes, if you have bad lung disease, or heart disease, etc., they can talk to you about the possible risks. Really, what it comes down to is how bad is a dental problem and how much is it affecting your life and your health? If there’s an infection, you know, that’s going to be really important to deal with, or an impacted tooth that has to come out, whereas we’re all for dental care and dental cleaning, but that can wait for right now. Yeah.
Elective medical procedures
Christine Herman: Dr. Clark, are you having similar conversations with patients who are wondering about non-emergency medical procedures and whether they should come in for those as well?
Dr. Ted Clark: That’s something that we’ve really been working on over the last two to three weeks, in terms of how to take care of our routine health issues in the age of COVID. And it’s really about living with COVID, knowing that we were prepared for an epidemic or a spike, but we also have to have business as usual.
Importantly, cancer screening is a great example. We’ll identify 20 cancers a month through our cancer screening programs, and those have been closed out for two months. And so as we open those back up, we’re counseling the patients on, yes, we’re doing everything we can to protect you so you can get in and get this very important service done.
Extend that into elective procedures. If people need an orthopedic procedure, if they’re suffering if they’re in pain, we’re again putting the processes in place through guidance, coming from the IDPH, to get these folks in and to get these procedures done. But we are having a lot of conversations around: Is this safe? Is this the right thing to do right now? And again, it’s just the slow stepwise opening of getting back to the new normal, and doing it carefully and doing it in such a way that if we do notice that there is an issue, or a spike, we can draw back if necessary.
Employer obligations
Christine Herman: Jay wants to know: “If multiple people at a job become ill with COVID-like symptoms, does the employer have an obligation to inform the employees?” Brandi, I know that there are guidelines for places like nursing homes and long-term care facilities, does the same thing apply to other employers as well?
Brandi Binkley: When we become notified of a positive case, and we conduct that contact tracing that we talked about earlier, we do contact that person, that is the positive confirmed case, and we asked them where they work. At that time, if it’s determined that there would been a risk of exposure to the workplace, then we do contact the workplace, and we do speak with someone that would be, you know, administration, a manager, an occupational nurse, and inform them of whom the person is so that we can determine, you know, what shifts have they worked? Have they completed home visits? Who has been in contact with them?
At that point, the employer is to notify the employees, but to do so with confidentiality. So they would notify the employees and say, you know, you may have been exposed to someone with COVID-19, you would not share the name with everybody in that place of employment.
And I think that’s a really important point. We’ve been asked, and we’ve seen a lot on social media about, why aren’t you telling us everywhere that it is? Why aren’t you giving us two people’s names or their address, etc.? And it’s very important that we maintain the privacy and safety of these people that are diagnosed with any communicable disease, including COVID-19. You know, things like privacy, safety, stigmatization that go with communicable disease, it’s very important that we maintain that privacy.
So it’s something that health departments do all the time when there’s communicable diseases. And that is what we are committed to doing ,to protecting that. So there is communication that occurs but a lot of it is very confidential. But we do have guidance that we do follow from IDPH that guides what we tell, when, and how that process should occur.
Christine Herman: Related to outbreaks at at work sites, Andrea wants to know: “Are all the cases in the count for Rantoul Foods included in the count for Champaign County?” Or do some of those cases live in other counties? Julie?
Julie Pryde: The cases are reported in the county that you live in. So if there were people working at Rantoul Foods who lived in another county, they would be counted in that county’s cases.
What’s on the horizon
Christine Herman: So as we wind down our discussion here tonight, we did get a question from Joseph: “When will it end?” This is a very difficult time for lots of people. Dr. Jokela, what do we know about what’s on the horizon?
Dr. Janet Jokela: That’s a really tough question. But I’m also really glad it was asked, because I think it’s really important in terms of how we think about it. There was an article in The New York Times within the last week or so that addressed this question, you know, how will it end, and you know, what’s that mean?
And in that article, they talked about two different things. One was sort of, scientifically and medically, when does it end? So when do we get on the backside side of the surge? When do we stop seeing new cases? That we don’t know and there’s a number of models out there for the maybe like little mini surges down the road. We really don’t know and so much also depends on work on a vaccine and effective treatments and all that.
The other aspect of it, and I don’t know if this is where the questioner was coming from, but kind of more socially, when does it end? And it gets back to what Dr. Clark was talking about, too. When do we move into this time of living with COVID and appreciating the risks, and how do we mitigate those risks, knowing it’s still out there? And I think those are two very different questions that, probably, we all have to answer in some way, shape or form.
And, again, I think public health is really beautifully situated to help inform the community and educate in terms of, you know, reopening isn’t like flipping a switch. It’s a very gradual thing and it doesn’t mean that social distancing and wearing masks suddenly gets turned off. This is going to be a very gradual process as we all move through this together.
Christine Herman: Even once there is a vaccine available, as many people are working on developing that on the research side, that’s still quite a ways away. Is that right, Dr. Healy?
Dr. Robert Healy: Yeah, it is. I’ve heard as others have various people and their crystal ball trying to figure out why this might happen. And I hope it happens quicker than what’s happened in the past, which is that it takes sometimes years to develop a vaccine.
I think we’ll be quicker this time. The technology is so much better. Within a week, we had the DNA sequencing of this virus, for instance, that was unheard of a couple of years ago. Hopefully we’ll get to to a vaccine soon. I do want to point out: Everyone needs to get vaccinated. We have a we have we have a vaccine for influenza every year. Nationally, 60% of us, only six in 10 get the vaccine. We should really make that 100% or close to it this fall.