A Spanish translation of this story is available here.
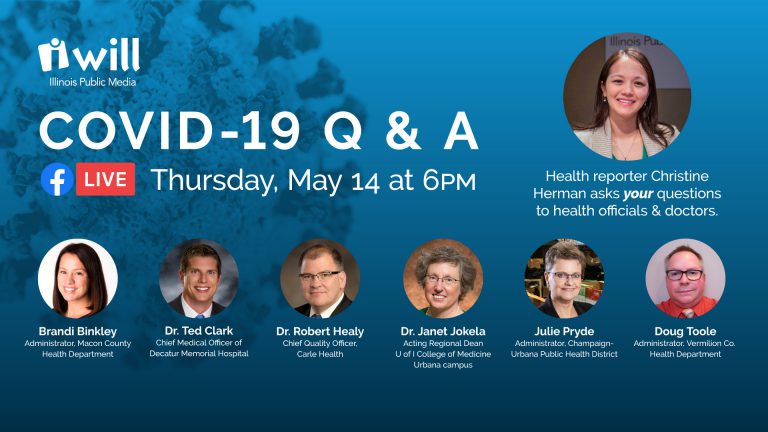
WILL and Illinois Newsroom hosted a “COVID-19 Q&A” Facebook Live discussion on Thursday, May 14, which gave people the opportunity to ask questions of our panel of local public health officials and medical experts.
Topics included:
- Status updates from local public health administrators and medical doctors
- COVID-19 immunity, contact tracing, social distancing and face mask guidance
- Antibody testing, advice on reopening the economy, questions about childcare
- Dental care, elective medical procedures, public health services and what’s on the horizon
- Employer responsibilities, where to report issues and final thoughts
If you have a question about COVID-19, you can submit it to Illinois Newsroom through our “Ask The Newsroom” site.
The following is a transcript of the event. The panel discussion has been lightly edited and condensed for clarity.
Our panelists tonight span three counties in east-central Illinois. We have three public health administrators:
- Brandi Binkley is with the Macon County Health Department
- Julie Pryde is with the Champaign-Urbana Public Health District
- Doug Toole is with the Vermilion Health Department
We also have three medical doctors joining us.
- Dr. Ted Clark is chief medical officer of Decatur Memorial Hospital — in Macon County
- Dr. Robert Healy is chief quality officer at Carle — based in Champaign County
- Dr. Janet Jokela is the acting regional dean of the U of I college of medicine Urbana campus
This is a very difficult time for many people, and we know there are a lot of questions and perhaps a lot of conflicting information online. We hope tonight’s discussion will help provide some clarity and get some of your questions answered with the local experts we have with us.
Status updates
Christine Herman: To start, I’d like to check in with each of the local public health administrators. How are things looking regarding the COVID-19 pandemic in your county?
Julie Pryde: We’re up to about 6700 tests done (in Champaign County, as of May 14) and we have a total of 333 cases, and 153 of those are active. So we have 153 people in isolation, and well over 500 in quarantine at this time. The good thing is we only have three that are hospitalized, and we have had since the start of the pandemic, a total of seven deaths.
Brandi Binkley: As of today (May 14), around 3 pm, we had 158 confirmed cases of COVID-19 (in Macon County). We are giving an update on Mondays and Fridays to our community as far as how many total tests have been done. On Monday it was a little bit over 1400.
We have had 51 people that have been released from isolation, 85 are currently on home isolation. Of course, there are more that are quarantined, six are hospitalized, and unfortunately we have had 16 of our residents with COVID-19 pass away. We are currently managing some outbreaks. We are very grateful for our health department team and also all of our community partners that have been so strong in this COVID-19 preparedness and response effort.
Doug Toole: We’re doing alright, Vermilion County is the smallest of the three health departments we’ve got represented tonight. We only have about 75,000 residents in our entire county. We’ve done about 1300 tests total. Of those, we’ve had 32 test positive, one of those 32 has passed away, unfortunately. More than half the folks who have tested positive and released from isolation, only 14 of them are still being home-isolated, none hospitalized at this time. And I’ve been kind of curious watching the results come in, about half the positive cases we’ve had have been people under the age of 30.
Christine Herman: Any idea why that’s the case?
Doug Toole: Not really sure. Ours is a county that kind of skews older, so it’s odd that a higher percentage of young people are testing positive. But the ones with the more serious symptoms tend to be older.
Christine Herman: And let’s do a check in with the hospitals. Dr. Ted Clark, you are at Decatur Memorial Hospital. How are things looking over there?
Dr. Ted Clark: Well, the last two months have been very busy. As we instituted social distancing, we worked with the policies and procedures to take care of the COVID patients. On the inpatient side at DMH, we have had 270 persons under investigation. We’ve had 47 COVID-positive patients. We’ve had, unfortunately, eight deaths, it’s a very severe illness. And we’ve had 39 recoveries. 
So we certainly have done it, we know how to do it, we know how to take care of COVID. Our current planning right now is around how we live with COVID, as we expand into this new world where we’re living with it over a longer period of time, but not necessarily worried about major surges. We’ve got the processes in place to protect our patients, to protect our healthcare workers.
On a slightly different note, I ‘ve been very impressed and I’m very grateful to our communities that have taken this very seriously and done what needed to be done to flatten the curve here to save our region from a dangerous spike that would overwhelm our local healthcare resources. And I hope that as we move forward with releasing or relaxing some of our social isolation, I hope that everyone keeps in mind the importance of maintaining social distancing. So we don’t find ourselves in an epidemic stage again.
Christine Herman: And Dr. Robert Healy, you’re with Carle, which is based in Urbana, but you’ve got locations all throughout central and downstate, Illinois. How are things going with the Carle Health System?
Dr. Robert Healy: Well, similar DMH, a few months ago, we were struggling to prepare for a large surge that luckily never came. And I think our communities are similar because, here as well, people have been really good at sheltering in place and maintaining social distancing, and now wearing masks. We’ve been able to bend the curve, like you said, Dr. Clark.
It’s been amazing to see the system throughout and our employees and our staff and visitors all kind of going along with this new reality of, you know, coming through to certain doors in the hospital, having questions being asked and screening for whether people are symptomatic or not, keeping an eye out for people who are sick and getting them to the right place.
Luckily, right now, we’re pretty much in a lull. We have three (COVID-19) patients in the hospital, and that’s the lowest we’ve had since this began. And we’re ready if there’s more, we think there will be a time when there’s another surge and we’re preparing for that. But we’re ready now, and as was mentioned, it’s the new normal now, we’re going to exist with COVID, just like we’ve existed with influenza for many years, and we’ll see ups and downs and we’ll adjust to it.
Christine Herman: And Dr. Jokela, as the Dean of the U of I College of Medicine Urbana campus, how are things going with you and with your students?
Dr. Janet Jokela: Thank you so much, Christine, and thank you so much for the opportunity to be here tonight with everybody. We’re really blessed to have wonderful colleagues here in Champaign-Urbana, and I just can’t speak highly enough for our community and the work that’s been done to kind of bend the curve, flatten the curve, and maybe stretch out the curve a little bit to alleviate, you know, potential, you know, real problems inside the hospitals.
Our students are getting ready to enter back into the clinical space. So we’re excited for them, and they’re excited as well. And we’ve been doing a lot of remote distance-learning and we really commend our faculty for stepping up and helping to organize all that and deliver that curriculum. And I think in the broader picture with the U of I campus, both in Champaign-Urbana, also Chicago, there’s a lot of, you know, really important discussions taking place around: How do we do this? How do we bring back students? And how do we do what we do safely and in a way that is beneficial and is really representative of the excellence that defines the U of I.