Laurie Ayala works out of an office deep in Northwestern Medicine’s Prentice Women’s Hospital in Chicago, IL. Whenever the small, black landline phone on her desk rings, she answers. This phone is home base for Illinois’ Perinatal Syphilis Warmline. Launched in November 2023, the phone line is designed to answer questions about perinatal syphilis from medical professionals across the state.
The phone line was started in response to a dramatic increase in Illinois – and nationwide – in congenital syphilis cases, which occurs when the syphilis infection is passed from mother to baby during pregnancy. There were roughly 4,000 babies born with syphilis in the United States in 2022 – in 2012, that number was 335.
The warmline acts as a triage center for questions about test interpretation, diagnosis and treatment. The perinatal syphilis warmline builds off of Illinois’ perinatal HIV hotline, which was started statewide in 2005. These phone lines are a familiar model to Ayala, who has been in public health for 18 years, and worked with the HIV hotline since it started.
“There’s nothing like being able to pick up a phone and get a recommendation on your specific patient’s situation,” Ayala said.
The reasons behind skyrocketing cases are multifactorial. Dr. Helen Cejtin is an OB-GYN at Chicago’s John H. Stroger Jr. Hospital. In November, she co-authored a Morbidity and Mortality Weekly Report for the Centers for Disease Control and Prevention looking at how COVID might have impacted congenital syphilis cases in Chicago. The first thing she points to is inadequate testing and prenatal care.
“You have a huge chunk that’s just someone not getting prenatal care,” says Cejtin. “So why is that happening? Were they … uninsured, they couldn’t get to a doctor, they were homeless, they had no transit?”
The CDC found that about 40% of people who gave birth to babies with congenital syphilis received no prenatal care.
There are also individuals who are getting diagnosed but are either not receiving or completing treatment. Early stage syphilis in a pregnant person can be treated with one injection of Bicillin L-A, a form of penicillin. For later stage syphilis, the recommendation is three injections at intervals of 7-9 days. To be considered effective, treatment needs to be initiated at least a month before delivery.
Medical professionals point to challenging commutes, needing to take time off work and a lack of access to childcare as big barriers to treatment for their patients.
The CDC found that about 90% of the 2022 cases might have been prevented by timely testing and treatment. These barriers to treatment and prenatal care mean that congenital syphilis has a disproportionate impact on marginalized communities.
Dr. Lynn Yee is an associate professor of obstetrics and gynecology at Northwestern University and the medical director of the warmline.
“It becomes concentrated in communities in which people are more underprivileged, less resourced in medical care,” she says. “In the United States, that disproportionately means people who are marginalized in other ways.”
Yee describes syphilis as syndemic – when two or more illnesses interact with each other – with poverty, structural racism and a lack of access to healthcare.
“It just really emphasizes how our society lets certain communities down over and over again – especially considering how treatable it is,” she says.
CDC data shows that babies born to Black, Hispanic and Native mothers mothers were up to 8 times more likely to have newborn syphilis in 2021 than those born to white mothers. Black babies in the U-S have double the mortality rate of white babies. And as far as demographics in terms of who’s accessing care – in 2020, Black mothers were twice as likely to receive late or no prenatal care as compared to white mothers.
Interpreting test results to diagnose syphilis and knowing what course of treatment to follow can be challenging for medical professionals who are unfamiliar with the disease. The warmline team hopes to act as a data center, answering questions, searching treatment records and trying to reduce the number of patients who slip through the cracks.
As for other solutions, experts call for increased screening and the potential use of mobile health units that could bring treatment directly to pregnant people. Dr. Yee also stresses the need for broad, policy based solutions.
“What you really need isn’t just treatment during pregnancy and public health systems focused on pregnancy, you need systems that help people be as healthy as they possibly can before they even get pregnant,” she says.
The Illinois Perinatal Syphilis warmline can be reached at 1-800-439-4079. It operates Monday to Friday, 8am – 4pm CT.
Curious about other public health news? Email us at shortwave@npr.org.
Listen to Short Wave on Spotify, Apple Podcasts and Google Podcasts.
Listen to every episode of Short Wave sponsor-free and support our work at NPR by signing up for Short Wave+ at plus.npr.org/shortwave.
Today’s episode was produced by Rachel Carlson. It was edited by Rebecca Ramirez. Rebecca also fact-checked alongside Indira Khera. Patrick Murray and Ko Takasugi-Czernowin were the audio engineers.
Transcript:
EMILY KWONG, HOST:
You’re listening to SHORT WAVE…
(SOUNDBITE OF MUSIC)
KWONG: …From NPR.
Hi, SHORT WAVErs. Emily Kwong here back in the host chair. I’ve been away for the last few months developing a new show about Asian American and Pacific Islander history. You will hear all about it in May. But in the meantime, I am so glad to be back with this team, kicking it with Regina Barber, as we bring you new discoveries, everyday mysteries and the science behind the headlines.
OK, I am joined today by Chicago-based journalist and former SHORT WAVE intern Indi Khera.
INDI KHERA: Hi, Emily.
KWONG: Hi. So Indi, you’re here to talk about some solutions to an emerging public health crisis in the United States – that being this big increase we’re seeing in syphilis cases among newborns. Tell me about that.
KHERA: Yeah. So in 2012, there were 335 babies born in the U.S. with syphilis, which is a sexually transmitted infection that, if left untreated, can cause serious complications. Babies born with syphilis can develop brain and nerve problems or even be stillborn in some cases. In 2022, there were almost 4,000 babies born in the U.S. with syphilis.
KWONG: OK, that’s a huge jump.
KHERA: Yeah, I know. And these newborns have something called congenital syphilis. That’s when the infection is transmitted from mother to baby during pregnancy. And the reasons behind the roughly 755% increase in cases over the last 10-ish years are complicated.
KWONG: Yeah. OK, we want to hear more about this. How did you first hear about this?
KHERA: It started with a press release from the Illinois Department of Public Health about this phone line that they were launching dedicated to congenital or perinatal syphilis. I really didn’t know much about syphilis as an STI, let alone the fact that, you know, it was impacting newborns and children.
KWONG: Tell me more about this phone line. What is it called?
KHERA: So it’s called the Perinatal Syphilis Warmline. It’s not technically a hotline because it’s not 24/7. You can call from Monday to Friday, 8 to 4. It was launched by the Illinois Department of Public Health and Community Partners back in November. It’s kind of like a one-stop phone line that people in the medical field across Illinois can call for guidance, building off a tradition of STI hotlines nationwide. It was sort of designed with the idea of an early intervention in mind because an early intervention in perinatal syphilis really matters. If a pregnant person gets tested and starts the appropriate treatment at least 30 days before delivery, their syphilis can largely be treated with penicillin, which is our oldest true antibiotic, but only if they’re tested and treated in time.
(SOUNDBITE OF MUSIC)
KWONG: So today on the show, why congenital syphilis cases are increasing around the country. And we meet the public health leaders in Illinois working fearlessly to help pregnant people and newborns. You’re listening to SHORT WAVE, the science podcast from NPR.
(SOUNDBITE OF MUSIC)
KWONG: All right, Indi, so where does this story start?
KHERA: Let’s start at Northwestern’s Prentice Women’s Hospital in downtown Chicago…
(SOUNDBITE OF BABY CRYING)
KWONG: …In Laurie Ayala’s office. Whenever the small black phone on her desk rings…
(SOUNDBITE OF MUSICAL PHONE RINGTONE)
KWONG: …She answers.
LAURIE AYALA: Perinatal Syphilis Warmline – may I help you?
KWONG: Laurie is the head administrator of the Perinatal Syphilis Warmline. She’s the one answering most of the calls they receive.
AYALA: There’s nothing like being able to pick up a phone and get a recommendation on your specific patient’s situation.
KHERA: The phone line is a familiar model to Laurie, who’s been in public health for 18 years and has worked on the state’s perinatal HIV hotline since 2005. That one is 24/7.
KWONG: This is so cool. So this is, like, a tried-and-true public health solution.
KHERA: Yeah.
KWONG: Let’s talk about the problem in more depth. What is behind this huge rise in perinatal syphilis around the country?
KHERA: Yeah, that’s kind of been described to me as the million-dollar question. And the factors that go into that are really complicated.
KWONG: OK.
KHERA: I talked to Dr. Helen Cejtin about this. She’s an OB-GYN at Stroger Hospital in Chicago. She’s worked there for about 30 years. She actually wrote an article for the CDC looking at how COVID might have impacted congenital syphilis cases in Chicago. The first big thing that she points to is inadequate testing in prenatal care. In Illinois, it’s a law that pregnant people are tested for syphilis in their first prenatal visit and in their third trimester. Most states do have laws that require some kind of prenatal screen for syphilis, but there’s a ton of variability between states and the number of screenings required, and the exact timing of those screenings. Those laws are also dependent on someone getting prenatal care. And according to Helen…
HELEN CEJTIN: You have a huge chunk that’s just someone not getting prenatal care. So why is that happening, right? Were they, you know, uninsured – they couldn’t get to a doctor, they were homeless?
KHERA: The CDC found that about 40% of people who gave birth to babies with syphilis received no prenatal care. And then there are people who are getting diagnosed but can’t complete the proper course of treatment. If someone is diagnosed in the early stage of syphilis, one penicillin shot might be enough. But if your syphilis is at a later stage, it’s recommended that you get three shots at intervals of seven to nine days. And to be considered effective, that treatment needs to get started at least a month before delivery.
KWONG: Oh, wow.
KHERA: And I heard about some really serious logistical hurdles to making that possible, like needing to miss work or take a really challenging commute or find somebody to watch your kids while you go and get your shots. One advocate I spoke to said that a lack of access to child care is actually a huge and sort of underdiscussed barrier to treatment here. The CDC found that, in the 2022 cases, timely testing and treatment might have prevented about 90% of them.
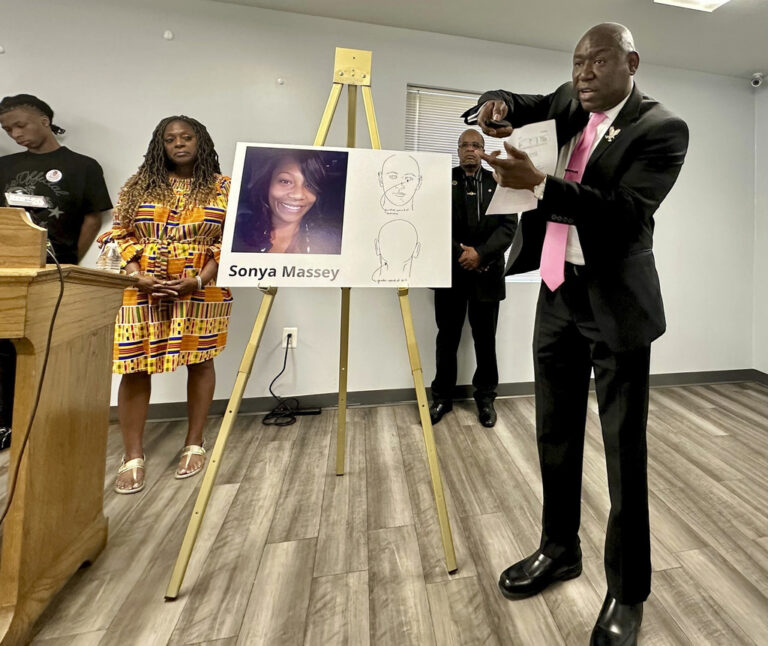
KWONG: That is significant. I mean, you’re basically saying that, to address this perinatal syphilis crisis, we have to think about health equity.
KHERA: Yeah.
KWONG: Right? Like, why it might be hard for someone to access health care and how to make it easier for them.
KHERA: Absolutely. Dr. Lynn Yee really underlined this for me when I talked to her. She’s an associate professor of obstetrics and gynecology at Northwestern, and she’s also the medical director of the warmline. And she brought up this idea of syndemics – pandemics that go together.
LYNN YEE: Like other infectious diseases, syphilis is a condition in which if you are exposed to other people with that infectious disease, you are more likely to have it. And so it becomes concentrated in communities in which people are more underprivileged, less resource to medical care. And in the United States, that disproportionately means people who are marginalized in other ways – people who are Black and brown and under-resourced from an income and insurance standpoint.
KHERA: CDC data shows that babies born to Black, Hispanic and Native mothers were up to eight times more likely to have newborn syphilis in 2021 than those born to white mothers. Black babies in the U.S. have double the mortality rate of white babies. And as far as demographics in terms of who’s accessing care, in 2020, Black mothers were twice as likely to receive late or no prenatal care as white mothers.
YEE: It just really emphasizes how our society lets certain communities down over and over again, especially considering how treatable it is.
KWONG: Yeah, that’s what surprises me – is you were saying earlier it is so treatable and also really wasn’t a huge problem a decade ago.
KHERA: Yeah. You know, Dr. Yee pointed to this kind of public health paradox that, when you pay really close attention to something and fund prevention, fund research, the disease kind of goes away. But then the funding goes away. And in the case of syphilis…
YEE: Over the last 10 to 20 years, we’ve really seen a lot less attention to syphilis in the perinatal space and in the general public health space. And as a result, there’s been a big rebound in syphilis.
KWONG: Oh, the great irony of public health.
KHERA: Yeah.
KWONG: The success stories are so invisible until there’s another problem.
KHERA: Yes, exactly. And, I mean, that brings us right to the next big thing, which is that the way COVID impacted public health systems is also a factor.
KWONG: Oh.
KHERA: Laurie talked about how, during COVID, because that was obviously such a crisis, a lot of public health people were redirected from STI prevention projects to COVID work. And then telehealth appointments, which became extremely common during the depths of the pandemic, made testing and detecting syphilis more challenging. And that’s not to mention that the public health workforce overall is grappling with serious shortages. I asked Helen what it felt like emotionally to be an OB-GYN working on this right now.
CEJTIN: Like, everything’s falling apart. Yeah. That’s what I would say. It feels like total disruption.
KWONG: Yeah. I mean, you can tell that she cares so much about these babies, these families.
KHERA: Yeah.
KWONG: And I think you’re giving us a really clear picture of all the different reasons why we see this rise in perinatal syphilis. You have the COVID pandemic, you have the unequal access to testing and treatment. How can a phone line actually make a difference?
KHERA: Yes. Yeah. And that was, like, my, I feel, like, core question through this whole thing. And what I learned is that syphilis is really, really challenging to diagnose.
KWONG: Oh.
KHERA: It’s described as the great imitator, and it can actually start in a pretty asymptomatic way. And then on the clinical side, interpreting test results is really challenging. So for doctors who haven’t been working in the infectious disease space, they might not have ever seen a case of syphilis. So basically, if you’re stuck on a test result or you can’t quite make a diagnosis, you can call the Warmline team up and get connected to an expert. They’ve gotten about 30 calls since November.
KWONG: Wow. OK.
KHERA: Yeah. And that’s just one way that it helps.
KWONG: What else does it do?
KHERA: They can help medical professionals find and administer the only safe treatment for pregnant people – a form of penicillin which is in shortage right now, which also helps prevent overtreatment.
KWONG: Wow. Yeah. Indi, this Warmline – it seems like something that other people, not just people in Illinois, could benefit from.
KHERA: Yeah. It’s definitely worth noting that Illinois is not one of the states getting hit the absolute hardest. That’s states like Mississippi and South Dakota. And Illinois was able to rely on a perinatal HIV public health infrastructure that already existed, which is not something every state can do. But experts I spoke to did talk about the opportunity for resource and knowledge-sharing nationwide across the existing tightly knit STI public health community.
KWONG: OK. And if you’re a person listening to this and you’re thinking about how to support moms and babies to turn the congenital syphilis crisis around, what can be done?
KHERA: Yeah. The one thing that I heard over and over again was screening, screening, screening, that clinicians in the emergency room, in primary care, need to enforce their state’s testing requirements and feel empowered honestly through things like the Warmline to diagnose and manage syphilis. Elizabeth Glaser is a public health nurse and the STI case manager for the Chinle Service Unit in the Indian Health Service. They serve the Navajo area. She brought up how the stigma around mental health and substance use disorder is kind of a critical part of this puzzle. Going back to our idea of syndemics, substance use disorder and syphilis can fit together in that way, too. And to treat this, we need to address both. And Dr. Yee stressed the importance, finally, of policy solutions like really strengthening mandatory case reporting and building out universal health care.
YEE: What you really need isn’t just treatment during pregnancy and public health systems focus on pregnancy. You need systems that help people be as healthy as they possibly can before they even get pregnant.
KWONG: Absolutely. Indi, thank you so much for this fantastic reporting.
KHERA: Thank you so much for having me.
(SOUNDBITE OF MUSIC)
KWONG: This episode was produced by Rachel Carlson and edited by our showrunner, Rebecca Ramirez. Indi Khera and Rebecca Ramirez checked the facts, and Patrick Murray and Ko Takasugi-Czernowin were the audio engineers. Beth Donovan is our senior director, and Collin Campbell is our senior vice president of podcasting strategy.
(SOUNDBITE OF MUSIC)
KWONG: I’m Emily Kwong. Thank you for listening to SHORT WAVE from NPR.
(SOUNDBITE OF MUSIC)