Rural hospitals aren’t just providers of medicine and health care, but also are often major employers and a massive part of a town’s tax base. However, mounting challenges are forcing these hospitals to merge and close in droves.
Since 2010, 95 rural hospitals have closed around the U.S., according to the North Carolina Rural Health Research Program, while 380 have merged between 2005 and 2016.
The American Hospital Association wants Congress to do something about it, and recently published a point-by-point overview of all the challenges rural health care systems face and what can be done.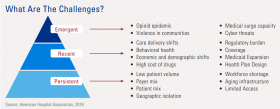
The troubles, according to the report, are a mixture of long-term problems (staff shortages, aging infrastructure), more recent problems (rising drug costs, federal regulation changes) and emerging problems, like the opioid crisis and cyber threats.
“Many rural hospitals, especially those with very limited resources, become overburdened as challenges intensify, accumulate, and compound each other,” the report stated. “Moreover, the issues of today may hinder rural providers’ preparedness for the challenges of tomorrow.”
Those problems are nothing new to David Schreiner, who’s the CEO of Katherine Shaw Bethea Hospital in Dixon, Illinois. He said employee wages and benefits, prescriptions costs and infrastructure upkeep are the biggest costs for his hospital, which was first built in 1897.
“Many rural hospitals especially are (operating) in buildings that were built a while ago,” he said, adding that the costs mount every year and with every change that’s needed to keep up with its aging clientele.
Both Schreiner and the report specifically pointed out how rural hospitals could use more reimbursement for their services. For example, the report states that in 2017, more than half of rural hospital revenue came from patients with Medicaid or Medicare — for which rural hospitals only get reimbursed about 87 cents for every dollar they spend.
Rural patients overall are also older, sicker and poorer than their urban counterparts.
Schreiner said many lawmakers from urban areas don’t understand what’s going on in rural hospitals, and rural hospitals can only shout so loud on their own.
While there’s been expert testimony in U.S. Senate committees and subcommittees in the past few months, the discussions often highlight more differences of opinion than a straightforward set of solutions.
U.S. Representative Cheri Bustos, a western Illinois Democrat, worked with rural health care networks for years before being elected to Congress. Just appointed to the House Appropriations Committee, Bustos said she wants to use her position to make sure rural hospitals have the funding they need.
She looked at the AHA report, and told Harvest Public Media that “it’s deeply concerning to me that nearly 100 rural hospitals have closed just since 2010.”
The report recommends expanding telehealth and health worker training, which Bustos said are “important,’ adding she plans to “work tirelessly to tackle these pressing issues for our rural communities.”
Even though hospitals have faced unique challenges for a while, the report said, “more recent and emergent challenges are exacerbating their financial instability — and by extension, the economic health of their communities.” One example given was the soaring costs of prescription drugs.
Overall, the authors of the report said that it’s up to the federal government to “play a principal role by updating policies and investing new resources in rural communities.”
Follow Madelyn on Twitter: @MadelynBeck8

