Physicians across the country have a message for the National Rifle Association: Gun violence is our concern. It’s part of a battle being fought vigorously on Twitter in recent weeks.
In late October, the American College of Physicians published a position paper in the Annals of Internal Medicine. The paper recommended a public health approach to gun violence and called for funding research, criminal background checks for gun purchases and other policies that it says could reduce firearm injuries and deaths.
On Nov. 7, the NRA said on Twitter that doctors had overstepped: “Someone should tell self-important anti-gun doctors to stay in their lane.”
And doctors responded in kind. Thousands of tweets from medical professionals and others poured in, many with the hashtags #ThisIsMyLane and #ThisIsOurLane. A new account, @ThisIsOurLane, has been active in promoting tweets about gun violence—even a video posted by a trauma surgeon showing a bullet being removed.
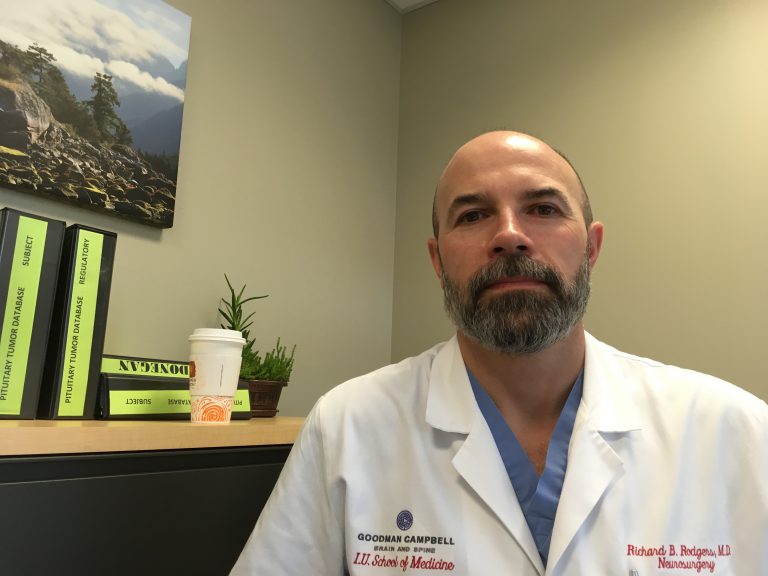
Dr. Ben Rodgers, assistant professor of neurological surgery at the Indiana University School of Medicine, has been outspoken about gun violence both before and after the NRA controversy. Side Effects spoke to him about the NRA controversy.
This interview has been edited for length and clarity.
What was your reaction to the NRA tweet when you saw it?
My reaction was, this is a medical problem. All the physicians that I know who take care of trauma patients or that work in emergency rooms strongly felt that they were well within their lane. This is exactly my lane. I see patients full of bullet holes all the time. This is where I belong. I have the right and the duty to advocate for prevention.
What do you see in your work as a neurosurgeon?
My role, if we have a patient with a gunshot wound to the head, is aggressive management of all of their normal bodily functions — airway, breathing, circulation. And the trauma surgeons are the ones aggressively helping with that. It’s one of the most devastating injuries you can have. Overall mortality is very high. The morbidity, as far as neurological deficits after such an injury, is incredibly high. Complication rates are terribly high. So they are difficult patients to manage.
And then the gunshot wounds to the spine, again, they’re neurologically devastating. Often patients with spinal cord injuries are quadriplegic or paraplegic, and we get several of those patients a year.
Can you tell me about a recent example where you know someone came in with an injury like that?
I’ve taken care of two police officers that were shot in the line of duty doing exactly what they’re supposed to do. Bad guy with a gun shoots the police officer. One of those cases, the officer died from his injuries. The other one made, I would say, a spectacular recovery — certainly markedly better than would be expected, but he still has neurological effects from his gunshot wound. It was one of the biggest events of my neurosurgical career.
How do these injuries affect doctors? Do doctors feel emotional effects from dealing with gun violence in the operating room or in the emergency room?
I think a lot of a lot of physicians are able to sort of shut off some emotion — some might describe it as being cold — at least to this specific event at the time, because our job is to do whatever damage control we need to do, and you can’t really get emotionally involved at the time.
If there’s emotion up front when we get called to the E.R. to see a gunshot wound, the first emotion I feel is a little bit on the angry side. It’s always some victim of violence or a victim of a crime. But it didn’t have to happen, right?
Here I am having a quiet evening of call or seeing other neurological things on call, and then this stupid thing comes in. It’s just senseless. I’m sure the trauma surgeons would say you know here I am taking care of a patient with a bunch of holes in his liver — again — when we should be doing something to prevent these kind of things.
Doctors obviously deal with the downstream effects of a lot of public health issues, and gun violence is one of them. When it comes to advocacy around an issue like gun violence, to the NRA’s point, why should we care what doctors think about the policy side of this debate?
Well, because gunshot wounds without a doubt are a medical problem. Physicians advocated for seatbelt laws and it turns out it’s a good thing because there’s fewer deaths in automobile accidents because people wear seatbelts now. What does a doctor know about how a car works?
If the physicians can’t advocate, at least on behalf of gunshot wound victims, then who’s going to?
Obviously, this controversy is still ongoing. Has this sparked action outside of Twitter?
Since this happened, the American College of Surgeons has put out their own recommendations on … common sense gun control. There were 20 some surgeons on a panel almost all of which were gun owners, and it was very similar to the other one.
There is a remarkable lack of funding for research into gun violence. So there’s a huge push to get that changed. These are things that take time, so I think we’re going to see something change over the course of the next year. It’s not going to be January but maybe the start of it will be coming in 2019. I don’t think this movement is going to die out.
I think the push has been growing. When the Parkland school shooting happened, there was this really vocal group of what seemed like really sharp kids. They spoke well and they’re still out there talking. And the NRA said some negative things about these silly kids. And that really got a lot of young people energized and they said, “You can’t talk about us like that.”
And here we are later. It feels like the NRA definitely pushed the wrong button and pissed off the wrong group of people. Physicians don’t like to be told what to do or what to not do. And I think everybody says that is exactly what we’re supposed to be. So I don’t think this issue for physicians is going to go away.
This story was produced by Side Effects Public Media, a reporting collaborative focused on public health.